Dengue
Dengue is an infection caused by the dengue virus of which there are four different subtypes. The disease is transmitted by mosquitoes

Key messages
-
Dengue is a viral disease spread by mosquitoes which predominantly feed during daytime hours.
-
Most people with dengue do not develop symptoms. When symptoms do occur, they can include high fever, muscle and joint pains, headache, nausea, vomiting and rash.
-
Most infections are self-limiting with improvement in symptoms and recovery occurring three to four days after the onset of the rash.
-
Severe dengue is a more serious form of the disease which is rare in travellers.
-
The number of reported cases of dengue in UK travellers has been increasing; most cases are acquired in Asia, Central and South America and the Caribbean.
-
Travellers should avoid mosquito bites. A vaccine is available in the UK; this is currently recommended only for those with previous dengue infection.
Overview
Dengue is caused by a virus of the genus Flavivirus, within the family Flaviviridae. It is spread by the bite of an infected Aedes spp. mosquito, which predominantly feed during daytime hours.
There are four distinct serotypes of dengue virus: DENV-1, DENV-2, DENV-3 and DENV-4. All have the potential to cause severe dengue, formerly known as dengue haemorrhagic fever (DHF). Severe dengue is more likely if a person has had a previous dengue infection.
According to the World Health Organization (WHO), the number of dengue cases reported worldwide has grown dramatically in recent decades. In 2000, there were 505,430 dengue cases reported to WHO, compared with 5.2 million in 2019 [1]. Factors associated with increasing risk of spread of dengue epidemic include climate change leading to increasing temperatures, high rainfall and humidity [2]. Other factors include the increased movement of people and goods, urbanisation and pressure on water and sanitation [3].
Under reporting, misclassification of disease and the practice of reporting confirmed cases only, means the global burden of disease is likely to be far greater: approximately half of the world's population is at risk, and it is therefore estimated that the likely incidence of disease is between 100-400 million infections each year [1].
Risk areas
Dengue occurs in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Dengue is endemic in more than 100 countries in Africa, the Americas, the Eastern Mediterranean, Southeast Asia and the Western Pacific, with Asia accounting for 70% of the global burden of disease [1].
Outbreaks of dengue are under-reported in Africa due to limited laboratory capacity and less well-developed dengue surveillance systems. However, the presence of the disease and the high prevalence of antibodies to dengue viruses in serological (blood test) surveys in local populations suggest that dengue virus infection is endemic in many parts of the continent [4].
Increasing global temperatures aid the wider geographic distribution of some species of Aedes mosquitoes. Temperate regions are therefore increasingly at risk of becoming endemic for dengue. Dengue-infected travellers returning from endemic areas can generate local outbreaks in areas where there are suitable mosquito vectors, even if dengue is not usually found in that region.
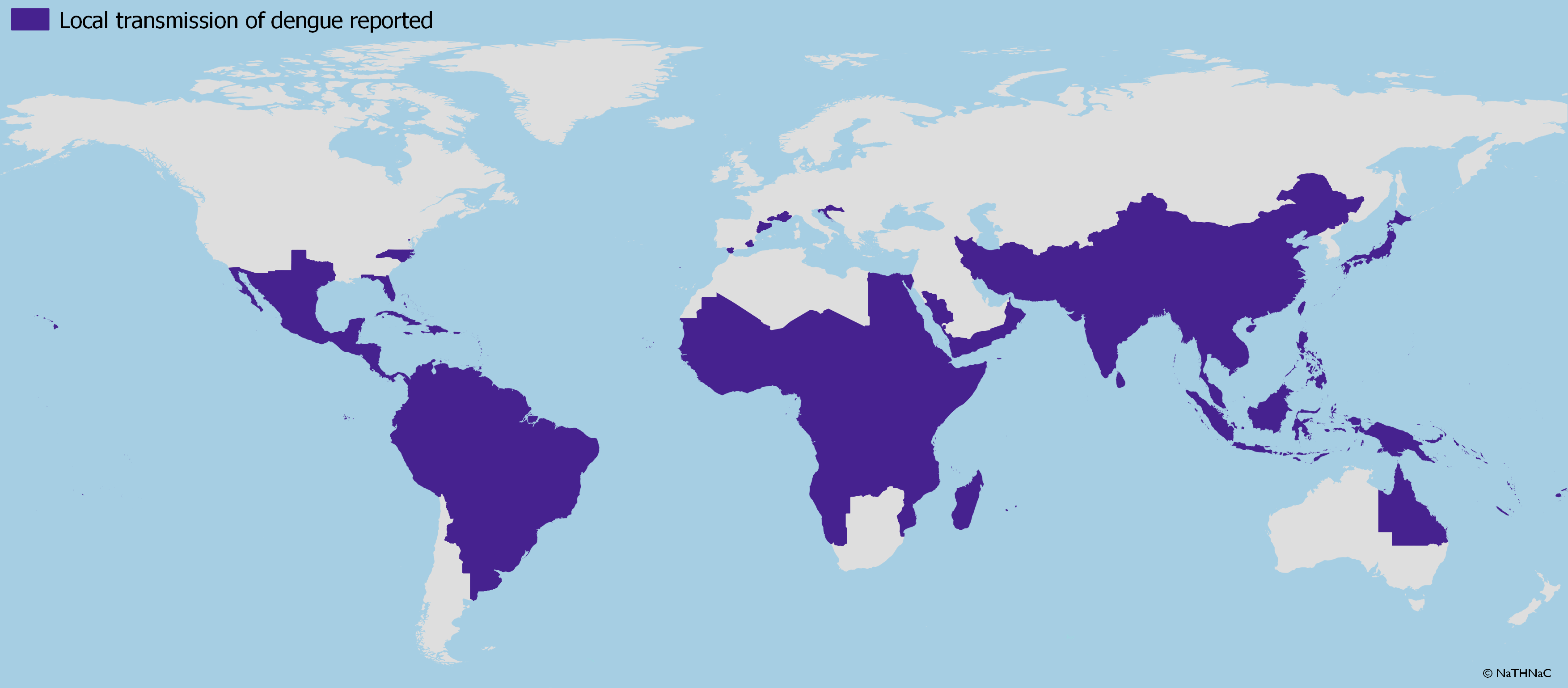
Dengue, countries or areas at risk, 2021
Schematic map illustrating where local transmission of dengue has been reported. Please see individual Country Information pages for up-to-date country details.
Dengue is now an emerging disease outside tropical areas, including parts of Europe [5]. Since 2010, several outbreaks have been reported in Europe in Croatia, France, Italy and Spain [6].
From September 2012 to March 2013, the autonomous Portuguese island of Madeira reported its first dengue outbreak, with 2,168 probable and 1,080 confirmed cases. Imported cases associated with this outbreak were also detected in travellers returning from Madeira to other countries in Europe, including the UK [7, 8].
Risk for travellers
The likelihood of contracting dengue is determined by several factors, including destination, length of exposure, intensity of transmission and season of travel [9, 10]. Risk is thought to be higher during periods of intense mosquito feeding activity (two to three hours after dawn and during the early evening).
All travellers to dengue endemic countries are at risk, although determining individual risk is difficult. True dengue incidence in travellers is probably underestimated as in many countries dengue reporting is not obligatory. Also, due to absent or non-specific symptoms, dengue is probably under-diagnosed [11].
Travellers who spend long periods in endemic areas (such as expatriates or aid workers) are at increased risk. However, even short-term visitors may be exposed [11-13].
Severe dengue is rare in travellers [14]. Individuals who are infected for the second time with dengue are at greater risk developing severe illness [1]. Severe dengue is also more common in children, adolescents, and pregnant women. An increased risk of severe disease has also been described in older individuals and those with comorbidities such asthma, diabetes, chronic renal failure, obesity, hypertension, bleeding disorders and in those taking anticoagulants [15, 16].
Dengue in UK travellers
Dengue does not occur naturally in the United Kingdom (UK) and it is a travel-associated infection. Most cases reported in returning UK travellers are acquired in Asia, Central and South America or the Caribbean. In 2023, a total of 634 cases of dengue (576 confirmed and 58 probable cases) were reported in England, Wales and Northern Ireland [14].
Information on dengue is available from UK Health Security Agency (UKHSA): laboratory confirmed cases reported in England Wales and Northern Ireland.
Transmission
Dengue is transmitted (spread) from human to human by different species of Aedes mosquito. Rarely blood-borne person to person transmission has been reported and pregnant women can pass the infection to their babies at the time of delivery [15]. Reports of sexual transmission are very rare [15, 17].
Aedes aegypti is considered the most efficient mosquito vector associated with dengue transmission and is closely associated with humans and their dwellings. A. aegypti mosquitoes breed in water containers (including buckets used to collect rainwater, cisterns, toilets and tyres) and rest inside in cool, dark rooms. In forests, they breed in water-filled tree holes [18]. They are most active during daylight hours, when they feed from dawn to dusk, but can bite at night in well-lit areas. A. aegypti requires higher, more tropical temperatures to survive.
Aedes albopictus mosquitoes also spread dengue [15]. Globally these mosquitoes are present in many areas including a number of European countries and are the vector most involved in spread of dengue in Europe [19]. A. albopictus is a relatively hardy species and can survive in cooler, more temperate climates.
Signs and symptoms
Approximately 40 to 80 percent of people infected with dengue have no symptoms [19]. When symptoms occur, illness begins abruptly after an incubation period of five to eight days. There may be high fever (up to 40°C), often accompanied by a severe headache and retro orbital (behind the eye) pain, muscle and joint pains, nausea, vomiting, abdominal pain and anorexia. High temperature can persist for two to seven days [19]. Around the third to fourth day, a maculopapular skin rash may be seen on the chest, trunk and extremities [15].
Health professionals should be alert to the warning signs of severe disease, which include easy bruising, bleeding in the gums or eyes, severe abdominal pain, liver enlargement and evidence of capillary leakage.
Severe dengue is characterised by bleeding, with major organ functions becoming compromised, resulting in respiratory distress, impaired consciousness and renal failure, and may ultimately lead to death [15, 20].
Diagnosis and treatment
The diagnosis of dengue can be confirmed by blood test (serology and viral detection) [21, 22].
There is no specific drug treatment for dengue. Management is supportive, aiming to alleviate symptoms and prevent complications. Most infections are self-limiting, with improvement in symptoms and rapid recovery occurring three to four days after the onset of the rash.
Patients may need to be admitted to hospital, with careful management of fever, fluid balance, electrolytes and blood clotting. Patients with severe disease may need to be admitted to specialist units such as intensive care or high dependencies units. With good supportive care, death due to severe dengue is typically less than one percent [15].
Anti-viral and steroid therapies have not been shown to aid recovery [15].
Long-term immunity to the infecting dengue virus serotype occurs in those who recover. However, infection with one serotype does not confer immunity to the other three serotypes or to other flaviviruses, and subsequent infection with a different dengue serotype may be more severe.
Health professionals should be alert to the possibility of dengue in those who have recently returned from a dengue risk area who present with a fever or flu-like illness [22, 23].
Clinical advice should be sought in the first instance from a local microbiology, virology or infectious disease consultant. Health professionals who suspect dengue should send appropriate samples for testing (with full clinical and travel history) to the UK Health Security Agency Rare and Imported Pathogens Laboratory.
The Imported Fever Service offers infection health professionals a 24-hour, seven day a week telephone access to expert clinical and microbiological advice for patients with suspected travel-associated infections, including dengue.
Preventing dengue
Prevention is by avoidance of mosquito bites. Particular vigilance with bite precautions should be taken around dawn and dusk. Those living in endemic areas should remove rubbish or water containers close to their home where possible as they can be breeding sites for mosquitoes.
Vaccine information
A vaccine, Qdenga®▼ has been licensed in the UK for the prevention of dengue disease in individuals from 4 years of age. The UK Joint Committee on Vaccination and Immunisation (JCVI) has advised that Qdenga®▼ vaccine can be considered for individuals aged 4 years of age and older who have had dengue infection in the past and are:
- Planning to travel to dengue where there is a risk of dengue infection or areas with an ongoing outbreak of dengue.
or
- Exposed to dengue virus through their work, for example, laboratory staff working with the virus.
Blood tests for previous dengue infection may not be 100 percent reliable [24] and assessment must be made of previous tests for dengue, likely exposure and clinical history, see Immunisation against infectious disease dengue chapter for further details on this and the use of Qdenga®▼.
Qdenga®▼ is a live vaccine (it contains live, attenuated dengue virus) and is contraindicated for anyone who is immunosuppressed, pregnant or breastfeeding. This vaccine is also contraindicated for those with hypersensitivity to any component of the vaccine and for children under four years of age [16, 25].
Another vaccine, Dengvaxia®, is not available in the UK but is licensed in some countries for use in endemic regions for use in at-risk people aged between 9 and 45 years of age. No interchangeability data are available, and travellers should not complete their Qdenga®▼ vaccine course overseas with Dengvaxia, and vice versa [16].
References
-
World Health Organization. Dengue and severe dengue. April 2024. [Accessed 22 October 2024]
-
World Health Organization. Disease Outbreak News. Dengue - Global situation. 21 December 2023. [Accessed 22 October 2024]
-
United Nations. Spike in dengue cases due to global warming, warns WHO. 23 July 2023. [Accessed 22 October 2024]
-
World Health Organization. Dengue: prevention and control. 2 April 2015. [Accessed 22 October 2024]
-
Rezza G. Dengue and other Aedes-borne viruses: a threat to Europe? Eurosurveillance Europe? Eurosurveillance 21:21. 26 May 2016. [Accessed 22 October 2024]
-
European Centre for Disease Prevention and Control. Autochthonous vectorial transmission of dengue virus in mainland EU/EEA, 2010 - present. Last updated 4 March 2024. [Accessed 22 October 2024]
-
European Centre for Disease Prevention and Control. Surveillance, prevention and control of dengue in Madeira: lessons learnt after the 2013 ECDC mission. 19 March 2014. [Accessed 22 October 2024]
-
Frank C, Höhle M, Stark K et al. More reasons to dread rain on vacation? Dengue fever in 42 German and United Kingdom Madeira tourists during autumn 2012. 4 April 2013. [Accessed 22 October 2024]
-
Jentes E, Lash R, Johansson et al. Evidence-based risk assessment and communication: a new global dengue-risk map for travellers and clinicians. J Travel Med. 13;23(6). 1 November 2016. [Accessed 22 October 2024]
-
Gautret P, Cramer J, Field V et al. Infectious Diseases among travellers and migrants in Europe. EuroTravNet 2010. Eurosurveillance 17:26. 28 June 201. [Accessed 22 October 2024]
-
Wilder-Smith A. Dengue infections in travellers. Paed International Child Health. 32:sup1, 28-32 12 November 2013. [Accessed 22 October 2024]
-
Massad E, Rocklov J, Wilder-Smith A. Dengue infections in non-immune travellers to Thailand. Epidemiol Infect. April 2012 24:1-6. [Accessed 22 October 2024]
-
Freedman D, Weld L, Kozarsky P et al. Spectrum of disease and relation to place of exposure among ill returned travelers. NEJM January 2006; 354:119-30. [Accessed 22 October 2024]
-
UK Health Security Agency. Travel-associated infections in England, Wales and Northern Ireland: 2023. Updated 21 March 2024. [Accessed 22 October 2024]
-
Jones N and Yacoub S. Dengue, Chapter 21 in Farrar, Jeremy, et al. Manson's Tropical Diseases. (24th edition). Elsevier - OHCE, 2023. Pg 202-211
-
UK Health Security Agency Dengue, Chapter 15a. Immunisation against infectious disease, October 2024. [Accessed 22 October 2024]
-
Lee C, Lee H. Probable female to male sexual transmission of dengue virus infection. Infect Dis (Lond) 2018:1-3. [Accessed 22 October 2024]
-
European Centre for Disease Prevention and Control. Communicable Disease Threats Report Week 45, 3-9 November 2019. Autochthonous dengue case-Spain-2019. [Accessed 22 October 2024]
-
European Centre for Disease Prevention and Control. Aedes aegypti - Factsheet for experts. Last updated 2 January 2023. [Accessed 22 October 2024]
-
Sánchez-González L, Adams L, Perez-Padilla J et al. Dengue. Section 5: Travel-Associated Infections & Diseases - Viral, In. Health Information for International Travel 2024. Centers for Disease Control and Prevention. [Accessed 22 October 2024]
-
World Health Organization and Special Programme for Research and Training in Tropical Diseases. Handbook for clinical management of dengue. November 2012. [Accessed 22 October 2024]
-
UK Health Security Agency (formerly Public Health England). Dengue fever: guidance, data and analysis. November 2015. [Accessed 22 October 2024]
-
Neumayr A, Muñoz J, Schunk M et al. Sentinel surveillance of imported dengue via travellers to Europe 2012 to 2014: TropNet data from the Dengue Tools Research Initiative. Eurosurveillance 22:1. January 2017. [Accessed 22 October 2024]
-
Joint Committee on Vaccination and Immunisation (JCVI). Draft Minutes of the meeting held on 7 February 2024. [Accessed 22 October 2024]
-
World Health Organization, Dengue vaccine position paper, September 2018, Weekly epidemiological record, 7 September 2018, 93, 457-476. [Accessed 22 October 2024]
-
Reference added to UKHSA dengue chapter in Immunisation against infectious disease, the 'green book' and updates to the vaccine information section.
Explore more
Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes
Updated: 12 February 2025Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosqu
Updated: 07 January 2025Influenza (flu)
Influenza is a highly infectious, viral infection of the lungs and airways
Updated: 18 December 2024Yellow fever
Yellow fever is caused by a virus, which circulates between infected monkeys or humans and mosquitoes
Updated: 17 October 2024Infectious diseases
Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes mosquito
Updated: 02 February 2018Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosquitoes
Updated: 13 February 2024Influenza (flu)
Influenza is a highly infectious, viral infection of the lungs and airways
Updated: 18 December 2024Preparing for healthy travel
Insect and tick bite avoidance
Protection from insect and tick bites is essential to help prevent vector-borne diseases such as malaria, yellow fever and Zika
Updated: 21 March 2024Travel Insurance
Travellers must declare medical conditions when taking out travel insurance to ensure they are suitably covered
Updated: 26 September 2019Special risk travel/traveller
Hajj and Umrah
The Ministry of Health of Kingdom of Saudi Arabia issue their requirements and recommendations for Hajj and Umrah annually
Updated: 15 May 2024Travelling with additional needs and/or disability
This factsheet provides an overview and advice on the points to consider when travelling with additional needs and/or disability
Updated: 06 February 2018Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Updated: 19 February 2021Clinic resources
Educational events
A list of courses, conferences and study days of relevance to UK health professionals working, or wishing to work, in the field of travel medicine
Updated: 14 March 2017Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines
Information for health professionals on availability of vaccines and use of unlicensed products
Updated: 17 October 2022The green book travel chapters
UK Health Security Agency Immunisation against infectious disease, the 'green book' travel chapter updates
Updated: 06 February 2024