Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Key messages
-
Travellers with sickle cell disease and some thalassaemias are at increased risk of infection.
-
Severe malaria is also a risk for these travellers. If travel is unavoidable, bite avoidance and strict adherence to anti-malarial prophylaxis is essential.
-
Any fever should be urgently evaluated due to risk of bacterial sepsis or malaria.
-
Travellers with sickle cell disease need to be aware of triggers for sickle cell crisis and know how to minimise the risks.
-
The risk of sickle cell crisis increases at altitude, when oxygen concentration in air is reduced. Travel to altitudes above 2,000 metres may trigger a crisis. During air travel, supplemental oxygen may be recommended for some.
-
Travellers carrying opioid pain medication may need to declare this to the airline and consult the destination country to ensure there are no entry restrictions.
Overview
Sickle cell disease (SCD) and thalassaemia are inherited red blood cell disorders, caused by the presence of an abnormal form of haemoglobin (oxygen transporting protein). According to the World Health Organization (WHO), approximately 5% of the world's population are healthy carriers of either of these genes [1].
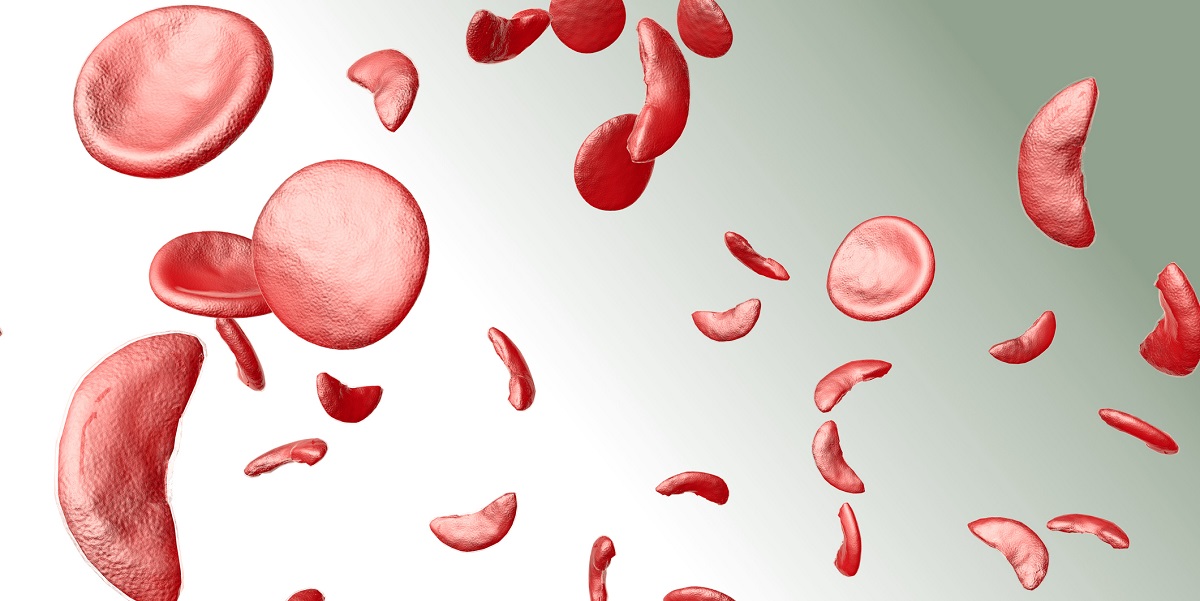
Sickle cell disease and sickle cell trait
Individuals with SCD have red blood cells that are 'sickle' shaped (like a crescent moon) instead of the normal 'doughnut' shape. SCD presents when the gene for sickle haemoglobin (HbS) is inherited from both parents. This is termed homozygous sickle cell disease (HbSS) or sickle cell anaemia [2]. This is the most common and severe type of SCD. Those who inherit a sickle cell gene together with a gene for normal haemoglobin (HbA), have sickle cell trait (also known as being a sickle cell 'carrier'). It is rare for sickle cell trait to cause health problems [2].
Sickle cell disease mainly affects those whose family origins are African or African-Caribbean.[2].
When oxygen is released into tissues, sickle cells change shape and stick together. Because of their shape they are unable to pass through small blood vessels, blocking the vessel and causing pain, usually in bones and joints. This can happen suddenly and be severe, lasting up to a week, causing symptoms known as sickle cell crisis. Triggers include the cold, lack of oxygen, dehydration, hard exercise, fever and infection [2]. Repeated blockages of blood vessels in, for example, the liver, kidney and spleen, can result in these organs being damaged. Those with SCD, particularly children, are also at increased risk of serious infections, mainly due to either partial failure of the spleen (hyposplenia) or complete failure (asplenia) [2].
Sickle cells are also removed from the body more easily than healthy red blood cells, often resulting in anaemia. Blood transfusions can decrease anaemia and reduce sickling temporarily [2, 3].
Treatment for sickle cell conditions involves the prevention and management of both infection and complications resulting from blockage of blood vessels. Stem cell transplant is the only available treatment that can cure SCD and is only used in severe cases [2]. To reduce the number of painful crises in those with SCD, hydroxycarbamide (hydroxyurea) may be recommended [2, 4]. However, hydroxycarbamide can have side effects and needs specialist monitoring [2].
Thalassaemia (alpha and beta) and thalassaemia trait
Thalassaemias are inherited conditions resulting in a reduced production of normal haemoglobin and the breakdown of red blood cells, leading to anaemia [5]. As a result, the body tries to produce more haemoglobin and red blood cells, which can cause additional complications [5].
Thalassaemias are classified as alpha and beta thalassaemias, according to which part (alpha or beta) of the haemoglobin is affected. Both alpha and beta thalassaemia are classified further according to severity of the condition e.g. major, intermediate or minor.
Beta thalassaemia major is the most severe type and causes severe anaemia, requiring regular blood transfusions and iron chelation therapy (removal of excess iron). In addition to anaemia, complications include iron overload (due to repeated blood transfusions), heart arrhythmias, hormone complications (leading to delayed puberty and restricted growth), liver disease and death [5]. The increased red blood cell production can result in enlargement of the spleen and reduced ability to control infections if challenged.
Treatment may be necessary for some beta thalassaemias, depending on severity of disease [5]. Stem cell or bone marrow transplant is currently the curative treatment option but is rarely performed [5].
Those with thalassaemia trait, who carry only one abnormal thalassaemia gene rather than two, may not have any symptoms or mild anaemia only.
Beta thalassaemia mainly affects people of Mediterranean, South Asian, Southeast Asian and Middle Eastern origin. Alpha thalassaemia is common in Southeast Asia, Africa and India [5].
Pre-travel preparation
Advice for those with SCD or thalassaemia should follow the usual advice given to all travellers, and tailored to the individual, considering severity of their illness, current treatment and medications. Assessment of a travellers' risk and the suitability of their destination and plans should ideally be discussed with a healthcare professional (and/or specialist) prior to booking. SCD and thalassaemia may be associated with reduced function of the spleen and will need to be assessed on an individual basis. For those with a dysfunctional or absent spleen, advice on the need for additional immunisations and antibiotic prophylaxis and standby treatment is available.
Destination specific risks and how to reduce risks can be found on the Country Information pages. Malaria is considered a significant cause of illness and death in those with SCD. Those with no spleen or severely impaired splenic function are also at particular risk of severe malaria. Where possible, travel to a malarious areas should be avoided [6].
Although little data is available, studies suggest that those with SCD can be at greater risk of medical complications when abroad [3]. Infection has been documented as the main hazard for children with SCD when travelling, primarily due to reduced function of the spleen [7]. However, both SCD and some thalassaemias are associated with an increased risk of infection for a variety of reasons, including splenic dysfunction; but also due to iron overload in those with thalassaemia [5]. Travellers should therefore ensure that any fever is urgently evaluated due to increased risk of bacterial sepsis and complications of malaria if infected.
In addition to the increased risk of infection, the main risk for adult travellers with SCD appears to be sickle cell crises (blockage of blood vessels) [3]. Travellers with SCD should be aware of the triggers for crises and know how to minimise the risks. They should also know where to access urgent medical care whilst abroad in the event of a sickle cell crisis or other complications. The Global Sickle Cell Disease Network lists researchers and clinicians worldwide working together to assist those with SCD.
Travellers should be aware that blood transfusions may not be reliable, nor available in many countries. Travel plans may need to be co-ordinated with transfusion schedules and iron chelation therapy in those with thalassaemia needing regular treatments.
Carrying a letter from a haematologist with the diagnosis and current drug treatment may be beneficial; this is particularly important if carrying opioid pain medications, which may need to be declared to the airline. Travellers should also determine if there are any restrictions on medications that can be carried into their destination country. Further information is available in the Medicines and Travel factsheet.
Travellers should also be advised to carry their own necessary medication, as substandard or falsified medication can be a problem in some countries.
Comprehensive travel insurance is essential for all travellers. A full declaration of medical conditions should be made to the insurers and all equipment, and planned activities should also be covered.
Journey risks
Flying
Sickle cell disease may be exacerbated by reduced oxygen pressures present in the air cabins. Because a crisis could be life-threatening, supplemental oxygen is sometimes recommended in-flight for those with SCD [8, 9]. This would need to be arranged with the airline prior to travel.
Sickle cell trait does not usually present a particular problem at normal cruising altitude in a pressurised aircraft, although there are rare reports of splenic infarction following air travel [10].
Travel should be deferred for at least 10 days following a sickle crisis and may need assessment by a clinician with aviation medicine experience and a medical assessment of fitness to fly [9, 10].
Severe anaemia should be corrected prior to air travel, and for those with a haemoglobin level less than 7.5g/dl, a medical assessment of fitness to fly would be needed, and oxygen considered in-flight [9].
Venous Thromboembolism
Prolonged air travel is a risk for venous thromboembolism (VTE) and studies from the WHO Research into Global Hazards of Travel (WRIGHT) project indicates that the risk of VTE approximately doubles after a long-haul flight (> 4 hours), and also with other forms of travel where travellers are seated and immobile [12]. Those with SCD are at increased risk of venous thromboembolic disease, therefore an individual assessment of risk factors for thrombosis is required for these travellers.
Travellers should therefore be advised on measures to prevent travel related VTE including maintaining mobility in-flight [13]. Additional information on reducing the risk of VTE can be found on the Venous Thromboembolism factsheet.
Food and water-borne risks
Travellers with SCD are more susceptible to developing hypovolaemia (a reduced volume of blood circulating in the body) because of disease of small blood vessels in the kidney [3, 14]. Hypovolaemia may be further exacerbated by sun or heat exposure, lack of access to safe drinking water and diarrhoeal disease. This in turn could lead to sickle cell crisis during travel. It is therefore essential to advise on making safe food choices during travel and to maintain adequate hydration.
Due to an increased risk of infection, those with SCD and some thalassaemias should also have a lower threshold for seeking medical attention for diarrhoeal illness [3].
After careful risk assessment, standby antibiotics to be used in the event of diarrhoea may be considered when travelling to high-risk countries [15, 16]. Further information can be found in the Travellers' diarrhoea factsheet.
Vector-borne risks
Babesiosis, a parasitic infection transmitted by ticks, can result in severe infection in those with an absent or dysfunctional spleen. Bacterial infection with Capnocytophagia and Pasturella (both associated with cat and dog bites) can also cause overwhelming infection in some of these travellers. Further information on specific vector-borne risks for travellers with SCD or thalassaemias and associated splenic dysfunction can be found in the Asplenia and Hyposplenia factsheet.Malaria
Malaria is considered a significant cause of illness and death in those with sickle cell disease, causing further destruction of red blood cells in addition to that due to sickle cell disease itself [6, 17]. It is therefore essential that travellers with sickle cell disease who visit countries / areas with a risk of malaria take rigorous mosquito bite avoidance measures.
Sickle cell trait confers some protection against malaria, although antimalarial prophylaxis would still be required for those visiting areas at risk for malaria [6].
Thalassaemia may provide protection against severe malaria, but there is no evidence that it prevents uncomplicated malaria [6].
Splenic function must also be considered for those with SCD and thalassaemia. For those without a spleen or if splenic function is severely impaired, then rigorous use of mosquito bite prevention measures and strict adherence to appropriate chemoprophylaxis (malaria tablets) is advised, even in low-risk malaria areas, where bite avoidance and awareness alone are recommended for other travellers [6]. For areas regarded as 'very low' malaria risk, antimalarials would not be advised but bite avoidance and awareness of risk would still apply [6].
COVID-19
Individuals who have conditions which may lead to splenic dysfunction (such as homozygous sickle cell disease and thalassemia major) are considered clinically vulnerable to COVID-19 and have been included in the groups to continue to receive COVID-19 vaccination in the UK (see Tables 2 and 3 in Chapter 14a, COVID-19 in Immunisation against Infectious Disease).
Travellers with splenic dysfunction should assess their individual circumstances, including medical facilities at their destination, and consider whether postponing travel would be appropriate. Further specific advice for those with haemoglobin disorders is provided by the British Society for Haematology.
All individuals should follow current UK recommendations to reduce their risk of catching COVID-19 and passing it on to others.
General guidance regarding risk assessment for travel during the COVID-19 pandemic and information about the COVID-19 vaccination programme is available.Vaccination
Those with SCD and thalassaemias should be up to date with routine immunisations and boosters as recommended in the UK. In addition, immunisations for those with splenic dysfunction need to be considered (i.e. pneumococcal, Men ACWY, Men B and influenza) [18]. Those receiving regular blood transfusions should be vaccinated against hepatitis B [19].
Sickle cell disease and thalassaemia alone are not considered a contraindication for vaccination [3]. However, as in all travel consultations it is important to consider any other underlying medical conditions, treatment or drug therapy which may contraindicate the use of live vaccines. Health professionals are encouraged to seek expert advice if further information is needed regarding use of live vaccines.
Other health risks
Altitude
For those with SCD, slight reduction in oxygen concentration at altitude can induce sickling. There is an increased risk of sickle cell crisis or splenic infarcts at altitudes above 2,000 metres. Travel to altitude should therefore be avoided in those with SCD [20].
Travellers with sickle cell trait and some thalassaemias (e.g. beta thalassaemia), are also at risk of crisis due to low oxygen concentration at high altitude. Splenic infarct has been noted at high altitudes in those with sickle cell trait, and severe exertion has also been associated with sickle cell crisis and sudden death in this group of individuals [20, 21]. Those with sickle cell trait who decide to travel to altitude should therefore be aware of the risks and advised to avoid over-exertion, maintain adequate hydration and to minimise heat stress [22, 23].
General advice for those who get sick abroad
Travellers should seek medical attention urgently if they have signs of infection (particularly fever), have had animal contact such as a bite, scratch or lick to an open wound, or a tick bite in a country with risk of tick-borne disease.
When seeking medical care abroad, travellers should inform health professionals if they have a dysfunctional spleen, together with other background medical information.
Resources
- NHS. Sickle Cell Disease
- Global Sickle Cell Disease Network
- NHS. Thalassaemia
- Thalassaemia International Federation
- British Society for Haematology
- GOV.UK: Coronavirus (COVID-19)
Patient Associations
References
-
World Health Organization, Regional Office for Africa. Sickle Cell Disease [Accessed 18 January 2021]
-
National Institute for Health and Care Excellence. Sickle cell disease. [Accessed 18 January 2021]
-
Willen SM, Thornburg CD, Lantos PM. The Traveler with Sickle Cell Disease. JTM 2014. Vol 21 (5); 1 Sept, 332-339
-
Qureshi A et al. Guidelines for the use of hydroxycarbamide in children and adults with sickle cell disease. A British Society for Haematology Guideline. Brit J Haem, 2018, 181, 460-475
-
NHS. Thalassaemia [Accessed 15 February 2021]
-
Chiodini PL, Patel D, Goodyer L. Guidelines for malaria prevention in travellers from the United Kingdom, 2023. London: UK Health Security Agency; July 2023 [Accessed 11 March 2024]
-
Sommet J, Missud F, Holvoet L, et al. Morbidity among child travellers with sickle-cell disease visiting tropical areas: an observational study in a French tertiary care centre. Arch Dis Child 2013; 98: 533-536
-
Aerospace Medical Association. Medical Considerations for Airline Travel [Accessed 18 January 2021]
-
Civil Aviation Authority. Guidance for health professionals: Haematological Disorders [Accessed 18 January 2021]
-
O'Shea J, Burke J, Murphy P, Quinn J. Splenic infarction in a young man with sickle cell trait following air travel at high altitude. Irish Medical Journal [Accessed 23 November 2020]
-
International Air Transport Association (IATA). Medical Manual, June 2018. 11th edition.
-
WHO Research into Global Hazards of Travel (WRIGHT) project, 2007, final report of phase 1
-
Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011: 152(1): 31-4,
-
Naik RP, Derebail VK. The spectrum of sickle hemoglobin-related nephropathy: from sickle cell disease to sickle trait. Expert Review of Hematology 2017; 10: 12; 1087-1094
-
Public Health England. Summary of antimicrobial prescribing guidance - managing common infections. PHE context, references and rationales for Clinical Commissioning Groups, Commissioning Support Units and Primary Care Providers. [Accessed 2 March 2020]
-
National Institute of Health and Care Excellence. Public Health England. Summary of antimicrobial prescribing guidance - managing common infections [Accessed 18 January 2021]
-
Bachmeyer C, Steichen O, Moreno-Sabater A et al. Cases of malaria in travellers with sickle cell disease - Chemoprophylaxis is important for this risk group. TMAID 2019; 35
-
UK Health Security Agency. Immunisation of Individuals with underlying medical conditions. Ch 7. In: Immunisation against infectious disease. January 2020 [Accessed 11 March 2024]
-
UK Health Security Agency. Hepatitis B. Ch 18. In: Immunisation against infectious disease. 4 February 2022 [Accessed 11 March 2024]
-
Pollard AJ, Murdoch DR. Introduction. The high altitude medicine handbook. 3rd Ed. Abingdon: Radcliffe Medical Press, 2003: 1-6.
-
Mieske K, Flaherty G, O'Brien T. Journeys to High Altitude - Risks and Recommendations for Travellers with Pre-existing Medical Conditions. JTM 2010: 17 (1); 48-62
-
Franklin QJ, Compeggie M. Splenic syndrome in sickle cell trait: four case presentations and a review of the literature. Mil Med 1999; 164: 230-233.
-
Le Gallais D, Bile A, Mercier J, et al. Exercise-induced death in sickle cell trait: role of aging, training, and deconditioning. Med Sci Sports Exerc 1996; 28: 541-544.
-
COVID-19 advice updated and content re-ordered.
Explore more
Mass gatherings
Travel advice for anyone planning to attend a mass gatherings event
Updated: 15 January 2025Travel and mental health
Travel health advice for travellers and health professionals
Updated: 02 November 2023Wildfires and industrial fires
Advice for travellers affected by wildfires or industrial fires during their trip
Updated: 28 January 2022Infectious diseases
Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes mosquito
Updated: 02 February 2018Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosquitoes
Updated: 13 February 2024Influenza (flu)
Influenza is a highly infectious, viral infection of the lungs and airways
Updated: 18 December 2024Preparing for healthy travel
Insect and tick bite avoidance
Protection from insect and tick bites is essential to help prevent vector-borne diseases such as malaria, yellow fever and Zika
Updated: 21 March 2024Travel Insurance
Travellers must declare medical conditions when taking out travel insurance to ensure they are suitably covered
Updated: 26 September 2019Special risk travel/traveller
Hajj and Umrah
The Ministry of Health of Kingdom of Saudi Arabia issue their requirements and recommendations for Hajj and Umrah annually
Updated: 15 May 2024Travelling with additional needs and/or disability
This factsheet provides an overview and advice on the points to consider when travelling with additional needs and/or disability
Updated: 06 February 2018Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Updated: 19 February 2021Clinic resources
Educational events
A list of courses, conferences and study days of relevance to UK health professionals working, or wishing to work, in the field of travel medicine
Updated: 14 March 2017Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines
Information for health professionals on availability of vaccines and use of unlicensed products
Updated: 17 October 2022The green book travel chapters
UK Health Security Agency Immunisation against infectious disease, the 'green book' travel chapter updates
Updated: 06 February 2024



