West Nile virus
Transmitted to humans by mosquitoes, the virus is present on every continent except Antarctica
Key messages
-
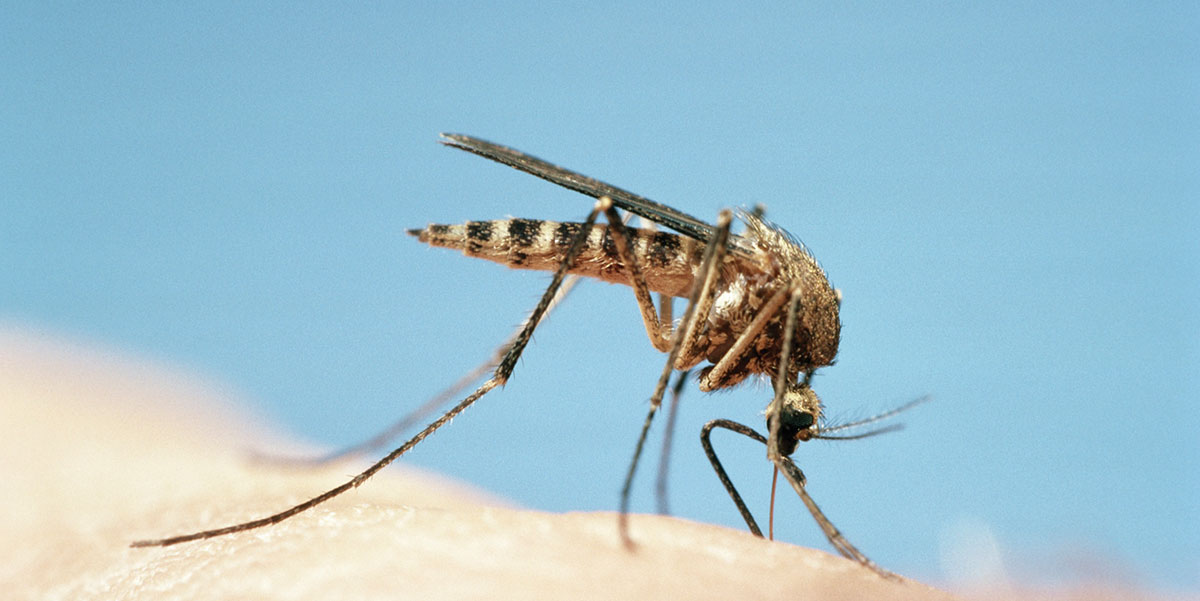
West Nile virus (WNV) is transmitted to animals, birds and humans by mosquitoes.
-
WNV infection is rare in United Kingdom (UK) travellers.
-
Most people who become infected with WNV do not have symptoms. Approximately 20 percent develop symptoms which may include fever, headache, tiredness, body aches, nausea, and skin rash.
-
Immunocompromised travellers, those over 50 years of age, and individuals with pre-existing medical conditions are at increased risk of developing severe illness.
-
There is no vaccine to prevent this disease in humans. Travellers should avoid mosquito bites day and night when visiting risk areas.
Overview
West Nile virus (WNV) is a mosquito-borne virus of the Flaviviridae family within the genus Flavivirus. WNV belongs to the Japanese encephalitis antigenic group of Flaviviruses, which includes Kunjin, Murray Valley and St. Louis encephalitis viruses. WNV is a zoonotic infection; a disease which can be passed from animals to humans.
WNV was first isolated from a woman with fever in the West Nile district of Uganda in 1937 [1]. Over the last 50 years, human infection attributable to WNV has been reported in many countries of the world.
Risk areas
The virus is present in every continent, except Antarctica, and is found in Africa, the Middle East, Asia and Australia (Kunjin virus). Outbreaks of WNV are also reported in several countries in Europe [2, 3].
The largest WNV outbreaks have occurred in Greece, Israel, Romania, Russian and the US, with outbreak sites on major bird migratory routes [4]. In 1999, the virus was first reported in New York and spread rapidly throughout the United States (US) subsequently causing a large outbreak (1999 to 2010) throughout continental US[4]. It has subsequently been detected in all US states, apart from Alaska and Hawaii [5]. Since its introduction to the US in 1999, the virus has spread widely and is now established in the Americas from Canada to Venezuela [4].In December 2014, the first human case of WNV was reported in Brazil [6].
WNV is now considered endemic in the US and Canada: State Health Departments monitor WNV activity during the transmission season in the US (which varies from State to State); maps showing WNV activity in the USA are available [7]. In Canada, surveillance for WNV is undertaken by Public Health Canada during the transmission season; maps showing WNV activity in Canada are available [8].
Outbreaks and intermittent cases of human WNV infection have also occurred in Europe since the 1950s. In recent years, human cases and outbreaks have been reported from Albania, Austria, Bulgaria, Croatia, Cyprus, Czechia, France, Greece, Germany, Hungary, Italy, Kosovo, Montenegro, North Macedonia, Portugal, Romania Serbia, Slovakia, Spain and Turkey [5, 9-13]. WNV transmission season in Europe is usually June to November [9, 10], but there are some indications that seasons may be lengthening; in 2018, the European transmission season was approximately nine weeks longer than usual [13].
Locally acquired WNV has not been reported currently in the UK [5, 10, 11]. However, in 2010, Culex modestus mosquitoes (the principal “bridge” vector responsible for WNV spread between birds, horses and humans) were found in the UK for the first time since 1944 [5].
The European Centres for Disease Prevention and Control (ECDC) carries out WNV surveillance during the transmission season in European Union (EU), European Economic Area (EEA) and EU neighbouring countries. ECDC also provide an interactive dashboard with maps showing countries reporting cases are available [2].
Risk in travellers
WNV risk is determined by length of exposure and intensity of transmission during travel to areas with WNV activity. Certain groups, including the immunocompromised (i.e. those with a reduced ability to fight infection), those over 50 years of age, and individuals with pre-existing medical conditions, are at increased risk of severe illness.
West Nile virus in UK travellers
WNV infection is rarely reported in UK travellers. Two confirmed imported WNV cases, acquired in South Africa, were reported in the UK in 2017. One other confirmed, imported acute WNV case has been reported in a returned UK traveller since 2012, with seven other clinically suspected cases showing compatible WNV serological test results [14]. It is possible that other cases with mild symptoms have not been reported or recognised as most WNV infections are asymptomatic (without symptoms) or produce mild symptoms.
Transmission
The main hosts of WNV are birds and the principal vectors are mosquitoes, predominantly of the genus Culex [15]. The virus is maintained in a mosquito-bird-mosquito cycle and in the mosquito population through vertical transmission (adults to eggs). Humans become infected when environmental conditions are favourable for mosquitoes and there are sufficient numbers of bird hosts. Culex spp. mosquitoes mainly bite in the evenings and at night. Humans, horses and occasionally other animals, become accidental hosts when bitten by an infected mosquito. Humans and animals serve as dead-end hosts (i.e. while becoming infected, humans and animals do not spread the infection) so there is no person-to-person transmission [4].
Peak WNV transmission season in temperate regions, such as Canada, North America and Russia, is late summer to early autumn when there is high mosquito activity. In tropical countries, transmission is year-round.
While exposure to infected mosquitoes remains the main risk factor for acquiring WNV, there have been isolated reports of non-mosquito spread occurring, such as transmission during blood transfusion and organ transplantation [4]. In 2012, UK NHS Blood and Transplant (NHSBT) screened 28,873 blood donors who had travelled to areas affected by WNV. Despite this travel history, no positive cases were identified [16].
Cases of infected pregnant women passing WNV on to their unborn babies, and a single probable case of a WNV infected mother passing the virus to her baby during breastfeeding, have also been described [17].
Signs and symptoms
The incubation period of WNV is typically two to six days, but ranges from two to -14 days, and can be up to 21 days in immunosuppressed people [15]. Most human infections (80 percent) do not cause symptoms (asymptomatic) [5, 15] or are very mild and go undiagnosed. Symptoms, if present, usually include a mild, self-limiting flu-like illness (West Nile fever) with fever, headache, myalgia (muscle pain) and a maculopapular (red and bumpy) rash. However, about one in every 150 cases progresses to a more serious neurological illness of meningitis (inflammation of the lining of the brain and spine), encephalitis (inflammation of the brain) or acute flaccid paralysis (when one or more limbs become weak or floppy). Those with neurologic disease may experience high fever, headache, neck stiffness, disorientation, muscle weakness, tremors, convulsions, flaccid paralysis and coma [5]. In these situations, the case fatality can be up to 17% [15]. Risk factors for severe illness include advancing age, underlying illnesses such as cancer, hypertension, kidney disease and genetic factors [5, 15].
Persistent neurologic complications have been observed in individuals who have survived acute West Nile encephalitis (WNE). Long-term movement disorders, cognitive complaints, and functional disability have been reported. WNE can result in an acute flaccid paralysis with a wide range of symptoms and degrees of limb weakness. These can range from mild monoplegia (paralysis of one limb) to flaccid quadriparesis (weakness or paralysis in all limbs) and acute neuromuscular respiratory failure. Facial nerve palsy (a condition causing weakness or paralysis of some face muscles) has also been observed [18].
Extreme tiredness is common after both WNV and WNE. In a study of 98 patients, 96 percent described post WNV fatigue, which lasted a median of 36 days [17]. Depression and personality changes have also been observed. Depression after encephalitis, regardless of etiology is not unusual: 31 percent of post WNV patients reported depression post-acute illness [19].
Immunity is considered to follow infection, although duration is unknown [13].
Diagnosis and treatment
There is no specific treatment for WNV.
Healthcare professionals should be aware of the signs and symptoms of WNV and be sure to obtain a travel history when assessing patients. Specialist advice must be sought when persons suspected of having WNV infection are evaluated. Information about diagnostic tests is available from the UK Health Security Agency (UKHSA). Appropriate serum and/or cerebrospinal fluid samples from suspect cases should be sent to the UKHSA Rare and Imported Pathogens Laboratory
WNV infection in animals and humans is notifiable to the relevant UK health agencies: UKHSA and Public Health Scotland, or for animal disease the Animal and Plant Health Agency (APHA) and Scotland: APHA Field Services. For suspected animal and bird cases in Scotland, see also: West Nile virus: how to spot and report the disease.
Preventing WNV
There is currently no vaccine to prevent WNV in humans. For travellers, prevention must focus on awareness of the risk of WNV in some destinations, plus mosquito bite avoidance measures.
Surveillance of human cases, together with monitoring of bird, animal and insect populations, are also essential steps in WNV prevention. Mosquito control programmes are important in areas where the virus occurs [7, 8, 15].
Resources
- European Centre for Disease prevention and Control: West Nile virus infection
- Insect and tick bite avoidance
- Government of Canada: Surveillance of West Nile virus
- UK Health Security Agency: Mosquito bite avoidance: advice for travellers
- UK Health Security Agency: West Nile virus epidemiology
- US Centers for Disease Control and Prevention: West Nile Virus
References
-
Smithburn K, Hughes T, Burke A, et al. A neurotropic virus isolated from the blood of a native of Uganda. Am J Trop Med Hyg 1940; 20:471-492.
-
European Centre for Disease Prevention and Control. Interactive dashboard. West Nile virus infections in EU/EEA and EU-neighbouring countries. [Accessed 7 October 2022]
-
European Centre for Disease Control and Prevention. West Nile virus infection – Annual Epidemiological Report for 2019. 19 March 2021. [Accessed 7 October 2022]
-
World Health Organization. West Nile virus. Factsheet. 3 October 2017. [Accessed 7 September 2022]
-
UK Heath Security Agency. West Nile virus epidemiology, diagnosis and prevention. Last updated 20 August 2018. [Accessed 7 October 2022]
-
World Health Organization. Disease Outbreak News. West Nile virus – Brazil. 15 December 2014. [Accessed 19 July 2022]
-
US Centers for Disease Control and Prevention. West Nile Virus: Statistics and Maps. [Accessed 7 October 2022]
-
Public Health Agency of Canada. West Nile Virus. 2 October 2016. [Accessed 7 October 2022]
-
European Centre for Disease Control and Prevention. Weekly updates: 2022 West Nile virus transmission season. Last updated 23 Sept 2022. [Accessed 7 October 2022]
-
European Centre for Disease Control and Prevention. Epidemiological update: West Nile virus transmission season in Europe, 2021. 24 March 2022. [Accessed 7 October 2022]
-
European Centre for Disease Control and Prevention. Surveillance Atlas of Infectious Diseases. West Nile virus infection. Locally acquired cases. Reported cases. 2020. [Accessed 7 October 2022]
-
Vlaskam D, Thijsen S, Reimerink J et al. First autochthonous human West Nile virus infections in the Netherlands, July to August 2022. Euro Surveill. 2020 Nov;25(46). [Accessed 7 October 2022]
-
Young J, Haussig J, Aberle S et al. Epidemiology of human West Nile virus infections in the European Union and European Union enlargement countries, 2010 to 2018. Euro Surveill. 2021 May;26(19):2001095. [Accessed 7 October 2022]
-
Parkash V, Woods K, Kafetzopoulou L et al. West Nile Virus Infection in Travelers Returning to United Kingdom from South Africa. Emerg Infect Dis. 2019;25(2):367-369. doi:10.3201/eid2502.172101. [Accessed 7 October 2022]
-
European Centre for Disease Control and Prevention. Factsheet about West Nile virus infection. 20 September 2018. [Accessed 7 October 2022]
-
Advisory Committee on the Safety of Blood and Organs. Position Statement: West Nile Virus and Solid Organ Transplantation. July 2013. [Accessed 7 October 2022]
-
Kramer LD, Linda M. Styer LM et al.. A Global Perspective on the Epidemiology of West Nile Virus. Ann Rev Entomol. 2008; 53:61-81. [Accessed 7 October 2022]
-
Sejvar J. The Long-Term Outcomes of Human West Nile Virus Infection. Emerg Infect 2007:44: 1617-1624
-
Murray K, Resnick M and Miller V. Depression after Infection with West Nile Virus. Emerg Inf Dis 2007:13; 3 [Accessed 7 October 2022]
Explore more
Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes
Updated: 12 February 2025Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosqu
Updated: 07 January 2025Influenza (flu)
Influenza is a highly infectious, viral infection of the lungs and airways
Updated: 18 December 2024Yellow fever
Yellow fever is caused by a virus, which circulates between infected monkeys or humans and mosquitoes
Updated: 17 October 2024Infectious diseases
Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes mosquito
Updated: 02 February 2018Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosquitoes
Updated: 13 February 2024Influenza (flu)
Influenza is a highly infectious, viral infection of the lungs and airways
Updated: 18 December 2024Preparing for healthy travel
Insect and tick bite avoidance
Protection from insect and tick bites is essential to help prevent vector-borne diseases such as malaria, yellow fever and Zika
Updated: 21 March 2024Travel Insurance
Travellers must declare medical conditions when taking out travel insurance to ensure they are suitably covered
Updated: 26 September 2019Special risk travel/traveller
Hajj and Umrah
The Ministry of Health of Kingdom of Saudi Arabia issue their requirements and recommendations for Hajj and Umrah annually
Updated: 15 May 2024Travelling with additional needs and/or disability
This factsheet provides an overview and advice on the points to consider when travelling with additional needs and/or disability
Updated: 06 February 2018Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Updated: 19 February 2021Clinic resources
Educational events
A list of courses, conferences and study days of relevance to UK health professionals working, or wishing to work, in the field of travel medicine
Updated: 14 March 2017Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines
Information for health professionals on availability of vaccines and use of unlicensed products
Updated: 17 October 2022The green book travel chapters
UK Health Security Agency Immunisation against infectious disease, the 'green book' travel chapter updates
Updated: 06 February 2024



