General Information
The information on these pages should be used to research health risks and to inform the pre-travel consultation.
Due to COVID-19, travel advice is subject to rapid change. Countries may change entry requirements and close their borders at very short notice. Travellers must ensure they check current Foreign, Commonwealth & Development Office (FCDO) travel advice in addition to the FCDO specific country page (where available) which provides additional information on travel restrictions and entry requirements in addition to safety and security advice.
Travellers should ideally arrange an appointment with their health professional at least four to six weeks before travel. However, even if time is short, an appointment is still worthwhile. This appointment provides an opportunity to assess health risks taking into account a number of factors including destination, medical history, and planned activities. For those with pre-existing health problems, an earlier appointment is recommended.
All travellers should ensure they have adequate travel health insurance.
A list of useful resources including advice on how to reduce the risk of certain health problems is available below.
Resources
Vaccine Recommendations
Details of vaccination recommendations and requirements are provided below.
All travellers
Travellers should be up to date with routine vaccination courses and boosters as recommended in the UK. These vaccinations include for example measles-mumps-rubella (MMR) vaccine and diphtheria-tetanus-polio vaccine.
Country-specific diphtheria recommendations are not provided here. Diphtheria tetanus and polio are combined in a single vaccine in the UK. Therefore, when a tetanus booster is recommended for travellers, diphtheria vaccine is also given. Should there be an outbreak of diphtheria in a country, diphtheria vaccination guidance will be provided.
Those who may be at increased risk of an infectious disease due to their work, lifestyle choice, or certain underlying health problems should be up to date with additional recommended vaccines. See the individual chapters of the 'Green Book' Immunisation against infectious disease for further details.
Certificate requirements
Please read the information below carefully, as certificate requirements may be relevant to certain travellers only. For travellers further details, if required, should be sought from their healthcare professional.
- There is a risk of yellow fever transmission in all areas of this country (see ‘Most Travellers’ section below).
- Under International Health Regulations, a yellow fever vaccination certificate is required from all travellers aged 9 months or over.
- According to World Health Organization (WHO), from 11 July 2016 (for all countries), the yellow fever certificate will be valid for the duration of the life of the person vaccinated. As a consequence, a valid certificate, presented by arriving travellers, cannot be rejected on the grounds that more than ten years have passed since the date vaccination became effective as stated on the certificate; and that boosters or revaccination cannot be required.
The yellow fever vaccine is not suitable for all travellers, there are specific undesirable effects associated with it. This vaccine is only available at registered yellow fever vaccination centres. Health professionals should carefully assess the risks and benefits of the vaccine, and seek specialist advice if necessary.
Most travellers
The vaccines in this section are recommended for most travellers visiting this country. Information on these vaccines can be found by clicking on the blue arrow. Vaccines are listed alphabetically.
Hepatitis A
Hepatitis A is a viral infection transmitted through contaminated food and water or by direct contact with an infectious person. Symptoms are often mild or absent in young children, but the disease can be more serious with advancing age. Recovery can vary from weeks to months. Following hepatitis A infection immunity is lifelong.
Prevention
All travellers should take care with personal, food and water hygiene.
Hepatitis A vaccination
As hepatitis A vaccine is well tolerated and affords long-lasting protection, it is recommended for all previously unvaccinated travellers.
Hepatitis A in brief
Tetanus
Tetanus is caused by a toxin released from Clostridium tetani bacteria and occurs worldwide. Tetanus bacteria are present in soil and manure and may be introduced through open wounds such as a puncture wound, burn or scratch.
Prevention
Travellers should thoroughly clean all wounds and seek medical attention for injuries such as animal bites/scratches, burns or wounds contaminated with soil.
Tetanus vaccination
- Travellers should have completed a tetanus vaccination course according to the UK schedule.
- If travelling to a country or area where medical facilities may be limited, a booster dose of a tetanus-containing vaccine is recommended if the last dose was more than ten years ago even if five doses of vaccine have been given previously.
Country-specific information on medical facilities may be found in the 'health' section of the FCDO foreign travel advice pages.
Tetanus in brief
Typhoid
Typhoid is a bacterial infection transmitted through contaminated food and water. Previous typhoid illness may only partially protect against re-infection.
Vaccination is recommended for most travellers, particularly travellers visiting friends and relatives, those in contact with an infected person, young children, frequent or long-stay travellers visiting areas where sanitation and food hygiene are likely to be poor, and laboratory personnel who may handle the bacteria for their work.
Prevention
All travellers should take care with personal, food and water hygiene.
Typhoid vaccination
- Oral and injectable typhoid vaccinations are available.
Typhoid in brief
Yellow fever
Yellow fever is a viral infection transmitted by mosquitoes which predominantly feed between dawn and dusk, but may also bite at night, especially in the jungle environment. Symptoms may be absent or mild, but in severe cases, it can cause internal bleeding, organ failure and death.
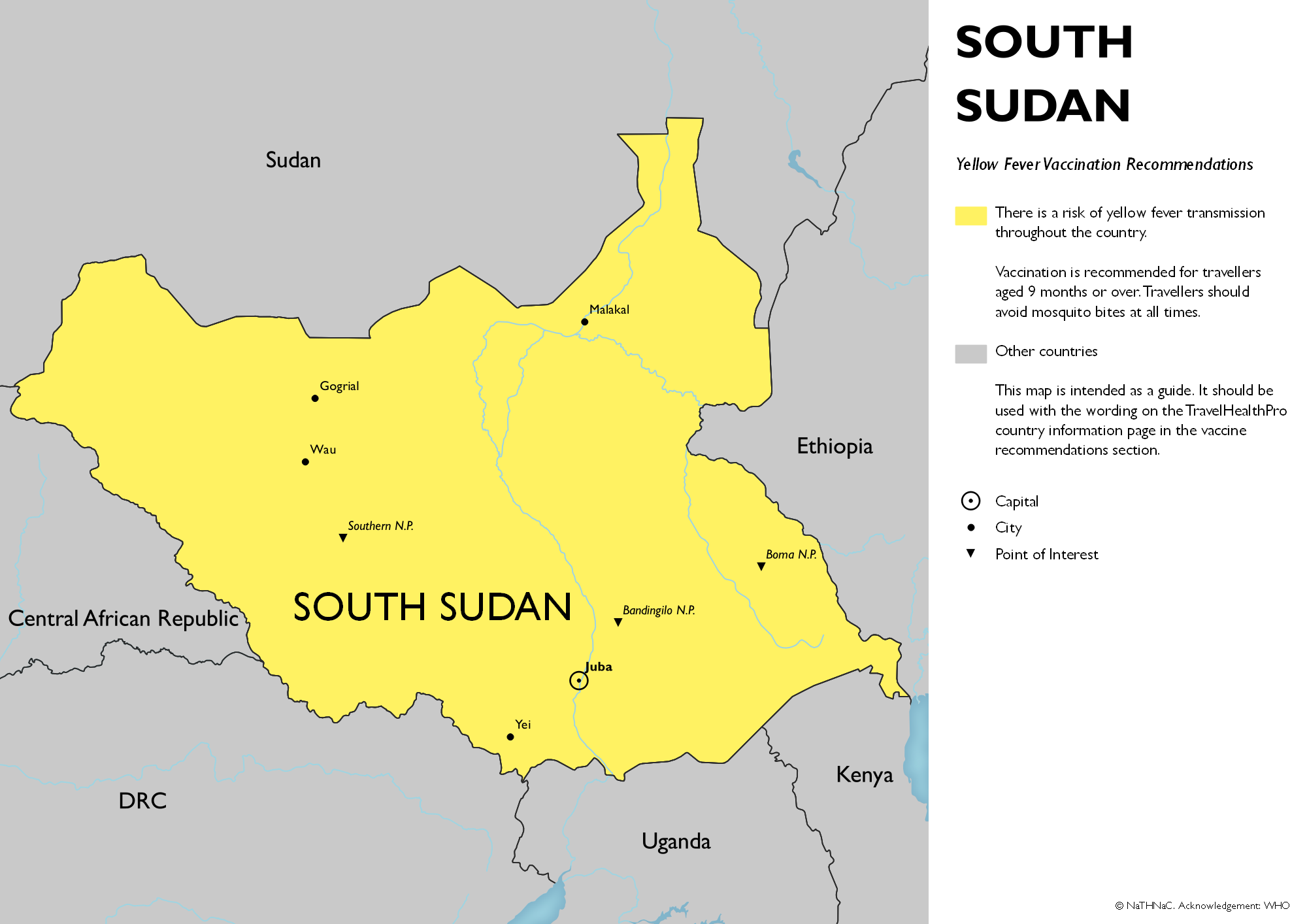
Yellow fever in South Sudan
There is a risk of yellow fever transmission throughout this country (see below).
Prevention
Travellers should avoid mosquito bites at all times.
Yellow fever vaccination
- Vaccination is recommended for travellers aged 9 months and older.
- See vaccine recommendation map below.
The yellow fever vaccine is not suitable for all travellers, there are specific undesirable effects associated with it. This vaccine is only available at registered yellow fever vaccination centres. Health professionals should carefully assess the risks and benefits of the vaccine, and seek specialist advice if necessary.
Yellow fever in brief
Yellow fever vaccine recommendation map for South Sudan
- Click on map to open in a new window
Some travellers
The vaccines in this section are recommended for some travellers visiting this country. Information on when these vaccines should be considered can be found by clicking on the arrow. Vaccines are listed alphabetically.
Cholera
Cholera is a bacterial infection transmitted by contaminated food and water. Cholera can cause severe watery diarrhoea although mild infections are common. Most travellers are at low risk.
Cholera in South Sudan
Cholera is presumed to occur in this country
Prevention
All travellers should take care with personal, food and water hygiene.
Cholera vaccination
This oral vaccine is recommended for those whose activities or medical history put them at increased risk. This includes:
- aid workers.
- those going to areas of cholera outbreaks who have limited access to safe water and medical care.
- those for whom vaccination is considered potentially beneficial.
Cholera in brief
Hepatitis B
Hepatitis B is a viral infection spread through blood, semen and vaginal fluids. This mostly occurs during sexual contact or as a result of blood-to-blood contact (for example from contaminated equipment during medical and dental procedures, tattooing or body piercing procedures, and sharing of intravenous needles). Mothers with the virus can also pass on the infection to their baby during childbirth.
Hepatitis B in South Sudan
This country is considered to have an intermediate or high prevalence of hepatitis B.
Prevention
Travellers should avoid contact with blood or body fluids. This includes:
- Avoiding unprotected sexual intercourse.
- Avoiding tattooing, piercing, public shaving, and acupuncture (unless sterile equipment is used).
- Not sharing needles or other injection equipment.
- Following universal precautions if working in a healthcare or other higher risk setting.
A sterile medical equipment kit may be helpful when travelling to resource poor areas.
Hepatitis B vaccination
Vaccination could be considered for all travellers and is recommended for those whose activities or medical history put them at increased risk. This includes:
- Those who may have unprotected sex.
- Those who may be exposed to contaminated needles through injecting drug use.
- Those who may be exposed to blood or body fluids through their work (e.g. health and aid workers).
- Those at high risk of requiring medical or dental procedures or hospitalisation e.g. those with pre-existing medical conditions, those who may require travelling for medical care abroad, or those travelling to visit families or relatives.
- Long-stay travellers.
- Those who are participating in contact sports.
- Families adopting children from this country.
Hepatitis B in brief
Meningococcal disease
Meningococcal disease is a bacterial infection transmitted by inhaling respiratory droplets or direct contact with respiratory secretions from an infected person. This is usually following prolonged or frequent close contact. The most common forms of meningococcal disease are meningococcal meningitis (infection of the protective lining around the brain) and septicaemia (blood poisoning).
Those at increased risk include healthcare workers, those visiting friends and relatives and long-stay travellers who have close contact with the local population.
Meningococcal disease in South Sudan
This country lies within the extended meningitis belt of sub-Saharan Africa.
Prevention
Travellers should avoid, if possible, overcrowded conditions.
Meningococcal disease vaccination
Vaccination is recommended for those whose activities or medical condition put them at increased risk including:
- healthcare workers
- those visiting friends and relatives
- those who live or travel ‘rough’ such as backpackers
- long-stay travellers who have close contact with the local population
- those with certain rare immune system problems (complement disorders) and those who do not have a functioning spleen
For travellers at risk, the ACWY conjugate vaccines are recommended.
Meningococcal disease in brief
Polio
Polio is caused by one of three types of polio virus and is transmitted by contaminated food and water. Previous infection with one type of polio virus does not protect against other types of the virus.
Those at increased risk include travellers who are unvaccinated or under-vaccinated visiting friends and relatives, those in direct contact with an infected person, long-stay travellers, and those visiting areas of poor sanitation.
This country is affected by circulating vaccine-derived poliovirus type 2 (cVDPV2).
Polio in South Sudan
Prevention
All travellers should take care with personal and food and water hygiene.
Polio vaccination
- All travellers should have completed a polio vaccination course according to the UK schedule.
- A booster dose of inactivated polio vaccine (IPV) is recommended for travellers to settings with extremely poor hygiene (e.g. refugee camps), or likely to be in close proximity with cases (e.g. healthcare workers), if they have not had a polio containing vaccination in the past 12 months.
- A booster dose of IPV containing vaccine should also be considered for immunosuppressed individuals travelling to an area with circulating vaccine-derived virus if they have not received a dose within the previous 10 years.
- According to the International Health Regulations, Emergency Committee, there is no polio certificate requirement for entering or leaving this country. If a live oral polio vaccine is offered to immunosuppressed travellers, their household contacts, pregnant individuals or others for whom live oral polio vaccine is contraindicated, this should be declined.
Polio in brief
Rabies
Rabies is a viral infection which is usually transmitted following contact with the saliva of an infected animal most often via a bite, scratch or lick to an open wound or mucous membrane (such as on the eye, nose or mouth). Although many different animals can transmit the virus, most cases follow a bite or scratch from an infected dog. In some parts of the world, bats are an important source of infection.
Rabies symptoms can take some time to develop, but when they do, the condition is almost always fatal.
The risk of exposure is increased by certain activities and length of stay (see below). Children are at increased risk as they are less likely to avoid contact with animals and to report a bite, scratch or lick.
Rabies in South Sudan
Rabies has been reported in domestic and wild animals in this country. Bats may also carry rabies-like viruses.
Prevention
- Travellers should avoid contact with all animals. Rabies is preventable with prompt post-exposure treatment.
- Following a possible exposure, wounds should be thoroughly cleansed and an urgent local medical assessment sought, even if the wound appears trivial.
- Post-exposure treatment and advice should be in accordance with national guidelines.
Rabies vaccination
Pre-exposure vaccinations are recommended for travellers whose activities put them at increased risk including:
- those at risk due to their work (e.g. laboratory staff working with the virus, those working with animals or health workers who may be caring for infected patients).
- those travelling to areas where access to post-exposure treatment and medical care is limited.
- those planning higher risk activities such as running or cycling.
- long-stay travellers (more than one month).
A full course of pre-exposure vaccines simplifies and shortens the course of post-exposure treatment and removes the need for rabies immunoglobulin which is in short supply world-wide.
Rabies in brief
Tuberculosis
TB is a bacterial infection most commonly affecting the lungs but can affect any part of the body. When a person with TB in their lungs or throat coughs or sneezes they could pass TB on to other people. TB is curable but can be serious if not treated.
The BCG vaccination helps to protect some people, particularly babies and young children who are at increased risk from TB.
Tuberculosis in South Sudan
This country has reported an annual TB incidence of greater than or equal to 40 cases per 100,000 population at least once in the last five years (further details).
Prevention
Travellers should avoid close contact with individuals known to have infectious pulmonary (lung) or laryngeal (throat) TB.
Those at risk during their work (such as healthcare workers) should take appropriate infection control and prevention precautions.
Tuberculosis (BCG) vaccination
BCG vaccine is recommended for those at increased risk of developing severe disease and/or of exposure to TB infection. See UK Health Security Agency Immunisation against infectious disease, the 'Green Book'.
For travellers, BCG vaccine is recommended for:
- Unvaccinated, children under 16 years of age, who are going to live for more than 3 months in this country. A tuberculin skin test is required prior to vaccination for all children from 6 years of age and may be recommended for some younger children.
- Unvaccinated, tuberculin skin test-negative individuals at risk due to their work such as healthcare or laboratory workers who have direct contact with TB patients or potentially infectious clinical material and vets and abattoir workers who handle animal material, which could be infected with TB.
There are specific contraindications to BCG vaccine. Health professionals must be trained and assessed as competent to administer this vaccine intradermally.
Following administration, no further vaccines should be administered in the same limb for 3 months.
The BCG vaccine is given once only, booster doses are not recommended.
Tuberculosis in brief
Malaria
Malaria is a serious illness caused by infection of red blood cells with a parasite called Plasmodium. The disease is transmitted by mosquitoes which predominantly feed between dusk and dawn.
Symptoms usually begin with a fever (high temperature) of 38°C (100°F) or more. Other symptoms may include feeling cold and shivery, headache, nausea, vomiting and aching muscles. Symptoms may appear between eight days and one year after the infected mosquito bite.
Prompt diagnosis and treatment is required as people with malaria can deteriorate quickly. Those at higher risk of malaria, or of severe complications from malaria, include pregnant women, infants and young children, the elderly, travellers who do not have a functioning spleen and those visiting friends and relatives.
Prevention
Travellers should follow an ABCD guide to preventing malaria:
Awareness of the risk – Risk depends on the specific location, season of travel, length of stay, activities and type of accommodation.
Bite prevention – Travellers should take mosquito bite avoidance measures.
Chemoprophylaxis – Travellers should take antimalarials (malaria prevention tablets) if appropriate for the area (see below). No antimalarials are 100% effective but taking them in combination with mosquito bite avoidance measures will give substantial protection against malaria.
Diagnosis – Travellers who develop a fever of 38°C [100°F] or higher more than one week after being in a malaria risk area, or who develop any symptoms suggestive of malaria within a year of return should seek immediate medical care. Emergency standby treatment may be considered for those going to remote areas with limited access to medical attention.
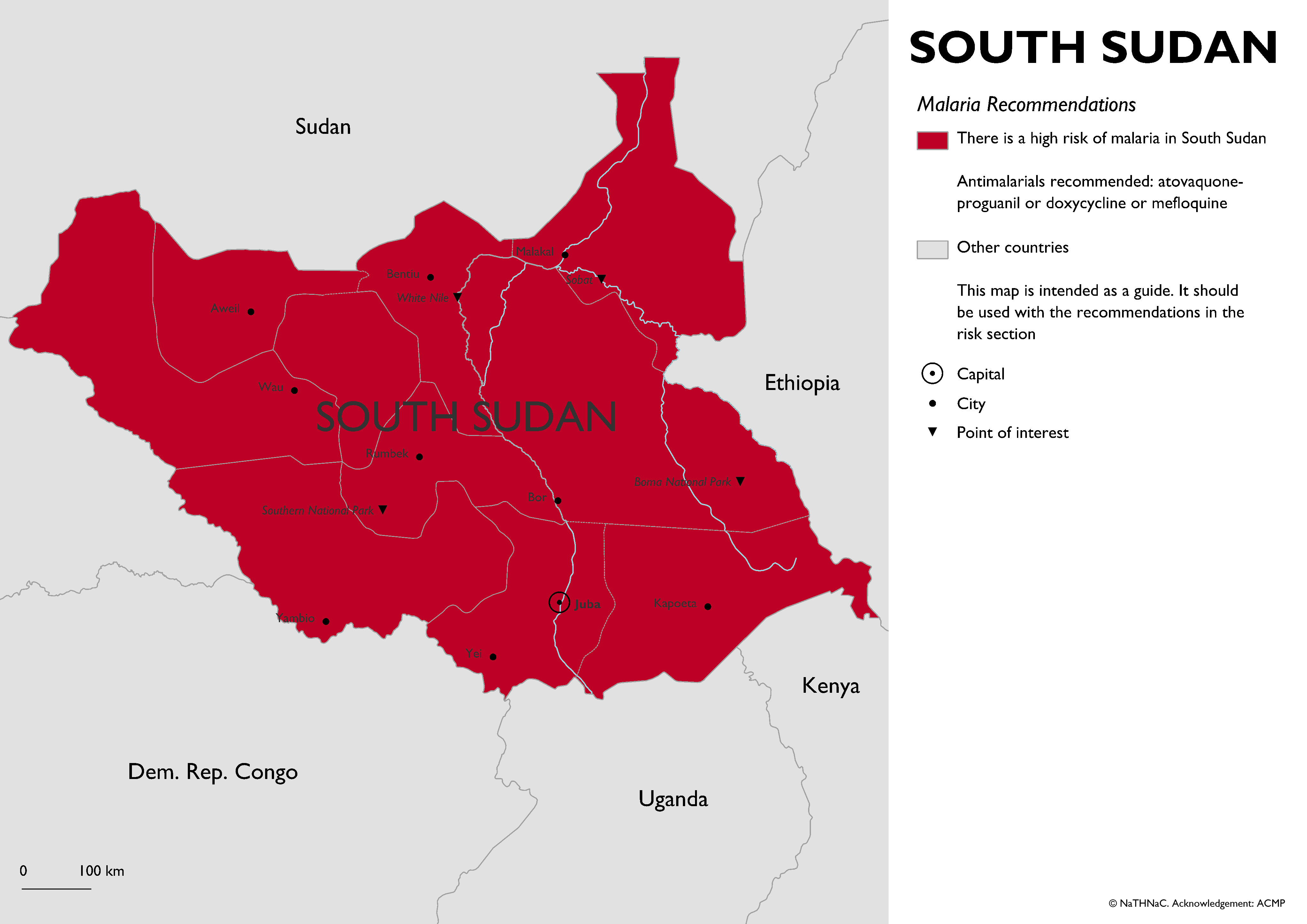
Risk areas
- There is a high risk of malaria in South Sudan: atovaquone/proguanil OR doxycycline OR mefloquine recommended.
Antimalarial recommendations map
- Click on map to open in a new window
Recommended antimalarials
The recommended antimalarials are listed below. If these are not suitable please seek further specialist advice.
Please note, the advice for children is different, the dose is based on body weight and some antimalarials are not suitable.
Atovaquone/Proguanil
Atovaquone 250mg/Proguanil 100mg combination preparation:
- start one to two days before arrival in the malaria risk area
- for adults, one tablet is taken every day, ideally at the same time of day for the duration of the time in a malaria risk area and daily for seven days after leaving the malaria risk area
- take with a fatty meal if possible
- for children paediatric tablets are available and the dose is based on body weight (see table below)
Doxycycline
Doxycycline 100mg:
- start one to two days before arrival in the malaria risk area
- adults and children over 12 years of age take 100mg daily, ideally at the same time of day for the duration of the time in a malaria risk area and daily for four weeks after leaving the malaria risk area
- take with food if possible; avoid taking this drug just before lying down
- not suitable for children under 12 years of age
Mefloquine
Mefloquine 250mg:
- this drug is taken weekly, adults take one 250mg tablet each week
- start two to three weeks before arrival in the malaria risk area and continue weekly until four weeks after leaving the malaria risk area
- for children the dose is based on the body weight (see table below)
Resources
Other Risks
There are some risks that are relevant to all travellers regardless of destination. These may for example include road traffic and other accidents, diseases transmitted by contaminated food and water, sexually transmitted infections, or health issues related to the heat or cold.
Some additional risks (which may be present in all or part of this country) are mentioned below and are presented alphabetically. Select risk to expand information.
Altitude
There is a risk of altitude illness when travelling to destinations of 2,500 metres (8,200 feet) or higher. Important risk factors are the altitude gained, rate of ascent and sleeping altitude. Rapid ascent without a period of acclimatisation puts a traveller at higher risk.
There are three syndromes; acute mountain sickness (AMS), high-altitude cerebral oedema (HACE) and high-altitude pulmonary oedema (HAPE). HACE and HAPE require immediate descent and medical treatment.
Altitude illness in South Sudan
There is a point of elevation in this country higher than 2,500 metres.
Prevention
- Travellers should spend a few days at an altitude below 3,000m.
- Where possible travellers should avoid travel from altitudes less than 1,200m to altitudes greater than 3,500m in a single day.
- Ascent above 3,000m should be gradual. Travellers should avoid increasing sleeping elevation by more than 500m per day and ensure a rest day (at the same altitude) every three or four days.
- Acetazolamide can be used to assist with acclimatisation, but should not replace gradual ascent.
- Travellers who develop symptoms of AMS (headache, fatigue, loss of appetite, nausea and sleep disturbance) should avoid further ascent. In the absence of improvement or with progression of symptoms the first response should be to descend.
- Development of HACE or HAPE symptoms requires immediate descent and emergency medical treatment.
Altitude illness in brief
Biting insects or ticks
Insect or tick bites can cause irritation and infections of the skin at the site of a bite. They can also spread certain diseases.
Diseases in Central Africa
There is a risk of insect or tick-borne diseases in some areas of Central Africa. This includes diseases such as African Trypanosomiasis (sleeping sickness), African tick bite fever, chikungunya, Crimean-Congo haemorrhagic fever, leishmaniasis, Rift Valley fever and West Nile virus.
Prevention
- All travellers should avoid insect and tick bites day and night.
- There are no vaccinations (or medications) to prevent these diseases.
Further information about specific insect or tick-borne diseases for this country can be found, if appropriate on this page, in other sections of the country information pages and the insect and tick bite avoidance factsheet.
Dengue
Dengue is a viral infection spread by mosquitoes which mainly feed during daytime hours. It causes a flu-like illness, which can occasionally develop into a more serious life-threatening illness. Severe dengue is rare in travellers.
The mosquitoes that spread dengue are more common in towns, cities and surrounding areas.
Dengue in South Sudan
There is a risk of dengue in this country.
Prevention
- Travellers should avoid mosquito bites particularly during daytime hours.
- A dengue vaccine is licensed in the UK for the prevention of dengue disease in individuals from 4 years of age. The Joint Committee on Vaccination and Immunisation (JCVI) and World Health Organization are in the process of reviewing the product information. Recommendations on the use of this vaccine will be published in due course.
Dengue in brief
Influenza
Seasonal influenza is a viral infection of the respiratory tract and spreads easily from person to person via respiratory droplets when coughing and sneezing. Symptoms appear rapidly and include fever, muscle aches, headache, malaise (feeling unwell), cough, sore throat and a runny nose. In healthy individuals, symptoms improve without treatment within two to seven days. Severe illness is more common in those aged 65 years or over, those under 2 years of age, or those who have underlying medical conditions that increase their risk for complications of influenza.
Seasonal influenza in South Sudan
Seasonal influenza occurs throughout the world. In the northern hemisphere (including the UK), most influenza occurs from as early as October through to March. In the southern hemisphere, influenza mostly occurs between April and September. In the tropics, influenza can occur throughout the year.
Prevention
All travellers should:
- Avoid close contact with symptomatic individuals
- Avoid crowded conditions where possible
- Wash their hands frequently
- Practise ‘cough hygiene’: sneezing or coughing into a tissue and promptly discarding it safely, and washing their hands
- Avoid travel if unwell with influenza-like symptoms
- A vaccine is available in certain circumstances (see below)*
*In the UK, seasonal influenza vaccine is offered routinely each year to those at higher risk of developing of severe disease following influenza infection, and certain additional groups such as healthcare workers and children as part of the UK national schedule (see information on vaccination). For those who do not fall into these groups, vaccination may be available privately.
If individuals at higher risk of severe disease following influenza infection are travelling to a country when influenza is likely to be circulating they should ensure they received a flu vaccination in the previous 12 months.
The vaccine used in the UK protects against the strains predicted to occur during the winter months of the northern hemisphere. It is not possible to obtain vaccine for the southern hemisphere in the UK, but the vaccine used during the UK influenza season should still provide important protection against strains likely to occur during the southern hemisphere influenza season, and in the tropics.
Avian influenza
Avian influenza viruses can rarely infect and cause disease in humans. Such cases are usually associated with close exposure to infected bird or animal populations. Where appropriate, information on these will be available in the outbreaks and news sections of the relevant country pages. Seasonal influenza vaccines will not provide protection against avian influenza.
Avian influenza in brief
Outdoor air quality
Poor air quality is a significant public health problem in many parts of the world. Exposure to high levels of air pollution over short time periods (e.g. minutes/hours/days) and longer time periods (e.g. years) is linked to many different acute and chronic health problems. These effects are mainly on the respiratory (lungs and airways) and cardiovascular (heart function and blood circulation) systems.
Current information on world air quality is available from the world air quality index project.
Prevention
Travellers with health problems that might make them more vulnerable to the effects of air pollution who are travelling to areas of high pollution should:
- discuss their travel plans with their doctor, and carry adequate supplies of their regular medication.
- take sensible precautions to minimise their exposure to high levels of air pollution.
- check local air quality data and amend their activities accordingly.
- take notice of any health advisories published by the local Ministry of Health and Department for Environment, and follow the guidance provided.
It is unclear if face masks are beneficial at reducing exposure and may make breathing more difficult for those with pre-existing lung conditions. Those who choose to use one should make sure that the mask fits well and know how to wear it properly.
Outdoor air quality in brief
Schistosomiasis
Schistosomiasis is a parasitic infection. Schistosoma larvae are released from infected freshwater snails and can penetrate intact human skin following contact with contaminated freshwater. Travellers may be exposed during activities such as wading, swimming, bathing or washing clothes in freshwater streams, rivers or lakes.
Schistosomiasis infection may cause no symptoms, but early symptoms can include a rash and itchy skin ('swimmer's itch'), fever, chills, cough, or muscle aches. If not treated, it can cause serious long term health problems such as intestinal or bladder disease.
Schistosomiasis in South Sudan
There is a risk of schistosomiasis in this country.
Prevention
- There is no vaccine or tablets to prevent schistosomiasis.
- All travellers should avoid wading, swimming, or bathing in fresh water. Swimming in adequately chlorinated water or sea water is not a risk for schistosomiasis.
- Drink water that is boiled, filtered or bottled.
- Application of insect repellent before exposure to fresh water, or towel drying after possible exposure to schistosomiasis are not reliable in preventing infection.
- All travellers who may have been exposed to schistosomiasis should have a health check to test for schistosomiasis infection.
Schistosomiasis in brief
COVID-19
COVID-19 disease is caused by the coronavirus SARS-CoV2. The main symptoms of COVID-19 are a new continuous cough, a high temperature, and a loss of, or change in, normal sense of taste or smell. Symptoms range from mild to life-threatening. Older people and those with underlying health problems are more likely to develop severe disease.
COVID-19 is spread through close contact with people who have the virus. It is mainly transmitted from person to person by breathing in droplets produced when someone infected with the virus breathes, speaks, coughs or sneezes. It is also spread by touching the infected droplets on surfaces, then touching the eyes, nose or mouth.
COVID-19 vaccines provide high levels of protection against severe illness, hospitalisation, or dying from the virus. Vaccination against COVID-19 reduces, but does not eliminate the risk of infection, so social distancing and personal and respiratory hygiene remain important interventions, particularly during overseas travel.
Travellers should always check the UK Foreign, Commonwealth & Development Office (FCDO) travel advice and their country-specific pages for the latest COVID-19 travel advisories which may include information on travel restrictions, quarantine, COVID-19 testing or vaccination requirements. This includes considering the recommendations and requirements for any transit countries.
Travellers should be aware that COVID-19 case numbers in individual countries/areas can increase rapidly, and healthcare capacity and country requirements can change at short notice.
COVID-19 in South Sudan
Most countries worldwide present a risk of exposure to COVID-19. The risk of COVID-19, public health policy, and travel advice or restrictions may change quickly, therefore travellers should ensure they have access to up to date information on COVID-19 and be prepared for rapid changes in guidance both before and during travel.
All travellers should check the FCDO travel advice and carefully consider their personal situation and risks of COVID-19 before travel to this country. This is particularly important in those at higher risk from COVID-19 who may wish to seek medical advice before travel.
Individuals entering or returning to the UK may be required to follow additional UK border measures.
Prevention
If travelling to this country, travellers should:
- Consider the risk at all destinations including any transit countries, and the risk during travel itself.
- Check with the airline/tour operator about preventive measures in place to reduce risk during travel.
- Follow the latest guidance on social distancing and face coverings, including any local requirements and maintain good hand, respiratory, and personal hygiene at all times. This may be particularly important if staying with friends and family.
- Ensure they are up to date with their COVID-19 vaccination courses and boosters as recommended in the UK vaccination programme.
See guidance on factors to consider when assessing the risk of COVID-19 for travellers.
If travellers develop COVID-19 symptoms while abroad, they should:
- Follow local guidelines on self-isolation, testing and avoiding travel.
- Contact their travel insurance provider.
- Seek medical advice if needed.
COVID-19 in brief
News
Mpox outbreak in Africa: clade I mpox virus infection
Mpox outbreak continues to meet the WHO criteria of a public health emergency of international concern (PHEIC)
Yellow fever update
Yellow fever cases continue to be reported in Africa and South America
Malaria: a reminder for travellers over the winter holiday season
Advice for travellers and health professionals about malaria
Outbreaks
Using information collated from a variety of sources, we regularly review and update information on overseas disease outbreaks and other health issues that may affect the UK traveller.
Please note that not all cases of disease or outbreaks are reported; some diseases may only be reported if they occur outside of the usual recognised risk area or season, or they have been reported in greater than usual numbers.
Further information on the Outbreak Surveillance section.
Cholera in South Sudan
On 22 January 2025, the World Health Organization reported that the current cholera outbreak in South Sudan has recorded 21,000 cases and 367 deaths. Cases have been reported in 31 out of 80 counties across seven states. Please see our Topics in Brief article for further details on cholera.
cVDPV2 in South Sudan
As of 18 December 2024, a total of nine cirulating vaccine-derived poliovirus type 2 (cVDPV2) cases have been reported in 2024. Please see our Topics in Brief article for further details on polio.
Malaria in South Sudan
The World Health Organization have reported an upsurge in malaria cases and deaths in most states between 1 January and 20 October 2024. Please see our Topics in Brief article for further details on malaria.
Western Bahr el-Ghazal state
Anthrax in South Sudan
As of 20 October 2024, a total of 162 human anthrax cases and 3 deaths have been reported in 2024. Cases have been reported from two States: Western Bar el Ghazal (87 cases) and Warrap (75 cases).